We only diagnose what we know and sometimes we need an X-ray vision
It is a universal truth in medicine and other sciences that investigate and interpret signs and symptoms. For us, clinicians, the signs and symptoms that the patient reports to us are clues that lead us in our medical, scientific and logical reasoning to the common thread that will allow us to associate our knowledge accumulated over decades of study and crystallized by our medical and surgical practice over the years and long hours of work with our patients.
On the other hand, our society evolves exponentially, scientific knowledge is nowadays much easier to obtain and distribute to the world’s knowledge centers with a speed that makes us feel small, slow and with limitations to keep up with the best and most current

Every day scientific articles are published on a certain topic in a certain area and it is with these contributions, smaller or greater than all added together, at the end of the day, they allow science to advance, they allow us doctors to follow this same advance and this symbiotic relationship between doctors and science, where both contribute to mutual success, that at the end of the process, the patients will be the big winners, and the doctor-patient relationship, the same one, which we learn and do everything to make it correct, balanced, fair, perfect and protected, will be tremendously enriched.
With this enormous technical and scientific evolution, we have gained in our daily clinical practice a new “arsenal” that allows us to be increasingly faster to diagnose, more correct to establish a treatment plan by priorities and severity and more predictable and safe in the treatments we offer as an option to our patients.
And these treatments tend to be more predictable, effective and efficient. And why?
By:
- Terms better means of diagnosis
- We work daily to enrich our training curriculum, from the medical, scientific, technical, radiological, computer and so on
- We can’t talk about surgery today, in my case
- Oral Surgery and Implantology, not to mention the digital and computer technology that helps us in surgeries.
This technology intervenes in:
- Diagnosis
- Planning
- Treatment
- Post-surgical control and maintenance.


When I have a patient for surgery, I start by establishing a Clinical History
In my opinion, there is no Medicine without Clinical History.
In the same way that we, as individuals, are a result of our stories and our experiences, the patient with his symptoms and the signs that we observe in the careful examination of the patient, intra-oral and extra-oral, is also ready to tell his story.
We have to know how to listen to the patient. Listen to and understand the stories and stories, those that may have a practical and direct reflection on the pathophysiology of the disease and the stories that are just to distract us, or at most to help the patient himself remember and fit the pieces of his own puzzle.
In terms of diagnosis, it is essential to have access to the best and most up-to-date diagnostic aids and this is something that the good practice of Oral Surgery and Implantology can never give up.
Here, in particular and in a very expressive way, Imaging gains contours of crucial importance, in its radiological aspect.



I have at my disposal, in my Clinics, current technology, “state-of-the-art technology” as it is now very fashionable to refer to
1 – Digital periapical X-ray with which we can detect and/or evaluate and measure:
- small lesions of the hard tissues in the region surrounding the tooth
- presence of dental caries
- Intra- and extra-radicular resorptions
- Proximal and distal bone defects in relation to each tooth
- Distance to relevant anatomical structures, such as nerves and anatomical cavities that cannot be injured, much less injured, with temporary or permanent clinical manifestations and complications
- Intraoperative and postoperative positioning of dental implants
- Inflammatory and infectious bone diseases
- Dental trauma
As a limitation, and speaking in general, we have the size of the intra-oral probe, which precisely because it enters the oral cavity, is of a reduced size and for this reason, the radiological image will also have smaller limits, not allowing us to evaluate more than 1 to 3 teeth and their surrounding areas at each radiation intake.
2- Panoramic X-ray, Digital Orthopantomography, which offers us an important diagnostic aid in various situations:
As the common name itself describes the function, the panoramic X-ray, the so-called Panoramic image, offers the Clinician who requests and studies it, a general image of the hard tissues, bones and teeth of the oral, nasal and antral cavity (maxillary sinus), as an example:
- It serves as a first diagnosis and a platform where a treatment plan begins to be built;
- Allows in just one 2D section (2 dimensions) to visualize at once all the dental parts in the mouth and their adjacent structures (periodontal ligament and alveolar bone);
- In terms of trauma, we can screen for a reasonable percentage of dental trauma (the first option being a periapical x-ray), trauma to the jaws, mandibular bone and maxillary bone, trauma to the temporomandibular joint (not being the 1st choice exam for this type of diagnosis);
- Granulomatous and cystic lesions of the hard tissues;
- Implant Surgery Planning.



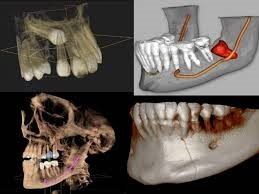
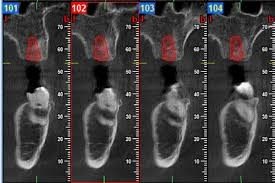
3 – C.B.C.T. – (Cone Beam Computed Tomography), which offers us the 3D study of anatomical structures and which arose with a need to present more reliable and precise information than a 2D exam such as Orthopantomography, but which in turn could emit less radiation than a conventional Tomography.
Allows:
- A more detailed and complete study for the planning of implant surgeries;
- A safer approach to tooth extractions next to noble anatomical structures, such as nerves;
- Rigor in measuring present and available bone dimensions;
- Virtual planning of surgeries with the possibility of placing implant models with their qualities and dimensions on the image;
- 3D reconstruction of images, for Oral and Maxillofacial surgery
In my clinical practice, patient safety always comes first, whether in the prevention of accidents, in biological contamination, the so-called cross-infection between patients and medical staff and between patients, and in the assessment and protection of radiological risk.
It all starts with the Clinical History and the collection of information on the patient’s health status and we avoid the use of radiation whenever possible, namely in pregnant women and children, respecting the specific “Guidelines” for the situation of both the General Directorate of Health (D.G.S.) and the Order of Dentists (O.M.D.).


Our Clinics are built according to the required requirements, have protective material for patients and employees, radiation meters and a strict radiological safety control by the competent authorities and audited by independent entities created for this function.
As I believe that our patients are increasingly interested and active in sharing therapeutic decisions, in the doctor-patient relationship, I also want to add in this article, a comparison of radiation between the different radiological exams.
The most current C.B.C.T. machines of the higher ranges, such as the one we have in our Clinic, allow a pulsed light emission instead of a continuous light emission, which to give you an idea:
- A scanner lasts between 5 and 40 seconds, depending on the type of scan and the area to be recorded. The more extensive the area, the longer the exposure time.
- For a 20-second scanner, we can have with an emission of a pulsed light beam, an exposure of 3.5 seconds only to radiation. (Whaites E, 2013)
The effective dose of radiation depends on:
- Amount and time of exposure;
- The size of the field of view, F.O.V. (the larger, the more radiation);
- The type of equipment used (modern digital equipment emits less radiation than old analog equipment);
- The anatomical location of the field to be irradiated and studied (Whaites E, 2013)
Examples of Radiation levels according to the type of Radiological Examination:
(Effective dose units – (E) mSv)
- Periapical Radiography – 0.0003 – 0.022;
- Panoramic Radiography – 0.0027 – 0.038;
- X-ray of the trunk – 0.014;
- X-Ray to Skull – 0.02;
- Computed Tomography;
- Head – 1.4;
- Abdomen Tomography – 5.6;
- Maxillary tomography – 0.25 – 1.4;
- dento-alveolar CBCT –0.01 – 0.67;
- CBCT Skull – facial – 0.03 – 1.1
(Whaites E, 2013)

As in everything in life, we have to know how to adapt and select for each clinical situation, the appropriate auxiliary means of diagnosis.
There is no perfect exam and proof of this is the need to sometimes have to request and do more than one.
But nowadays, with the technology we have at our disposal, we contribute to an increasingly predictable, effective and safe clinical practice, and the possibility of being able to plan our Surgical interventions virtually, allows me as a Surgeon to be increasingly safe, confident and happy with the technology that helps us in our daily work, both in my area of Oral Surgery and Implantology, as well as in the virtual planning of Oral Rehabilitation.
But I only talk about what I know, and leave it to my colleagues, to talk about their specific areas.
This is the beauty and safety of teamwork, and we at CERO Clinics do not give up both.
I end by thanking you for your time and attention with this text of mine.
See you soon and don’t forget to be happy. Despite everything, smiling doesn’t hurt.
If this is the case, if smiling causes you pain, nausea, or imbalance, consult your dentist.
Until the next opportunity!